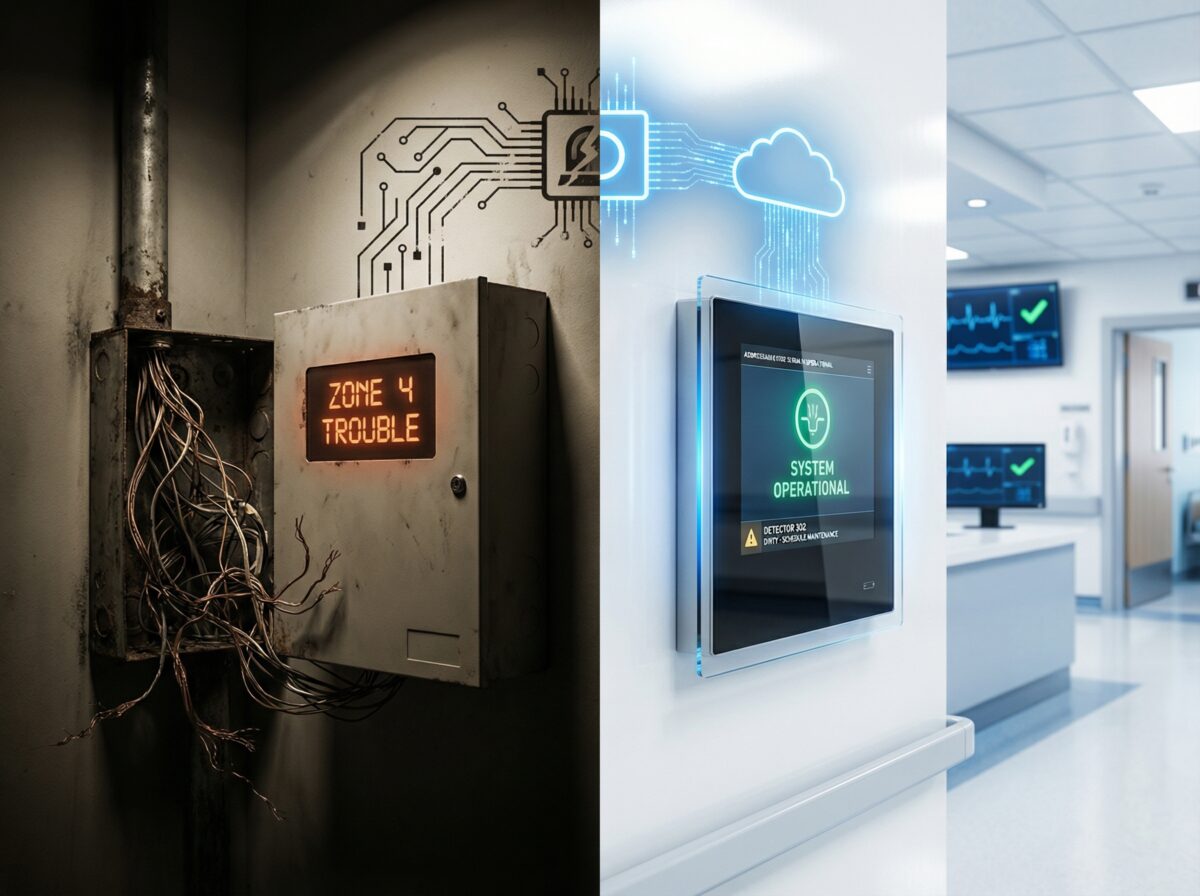
From Old Wiring to Cloud Alerts: One Hospital’s Alarm Story
Before: The Problem Emerges
Spring 2019
Facilities director receives third trouble call this month.
Panel display: “Zone 4 Trouble.”
Zone 4 contains: North wing second floor. Approximately 40 rooms. 60+ detection devices.
Which device has the problem? Unknown.
Technician arrives. Spends four hours checking devices one by one. Finds loose wire connection on smoke detector in vacant patient room. Repairs connection. Documents service call: $480.
Two weeks later: “Zone 4 Trouble” again. Different device, same zone. Another service call. Another $480.
The Accumulating Evidence
System age: 23 years. Installed 1996 during hospital expansion.
Technology: Conventional (zone-based). Four-wire smoke detectors. Coded horn notification.
Annual maintenance costs (trending):
- 2016: $3,200
- 2017: $4,800
- 2018: $6,400
- 2019 (projected): $8,500
Trouble frequency:
- 2016: 8 troubles annually
- 2017: 14 troubles
- 2018: 22 troubles
- 2019: 31 troubles (first 9 months)
False alarms:
- 2016-2017: 2 per year
- 2018: 5
- 2019: 8 (through September)
The Incident That Changed Everything
October 2019, 2:47 AM
Fire alarm activates. Zone 7: Kitchen area.
Security responds. No visible fire. No smoke. Calls fire department per hospital protocol.
Fire department arrives. Investigates kitchen thoroughly. No fire found. Alarm origin unclear—zone contains kitchen, adjacent storage, mechanical room, corridor.
False alarm logged. Fire department departs.
Cost of this false alarm:
- Fire department response: No charge (public service)
- But: Hospital now at 9 false alarms for year
- Jurisdiction threshold: 8 false alarms annually before fines begin
- Next false alarm: $500 fine
3:15 AM, same night
Zone 7 activates again. Different trouble pattern. Intermittent activation.
Fire department returns. Still no fire. Zone 7 placed out of service temporarily until technician arrival.
Risk: Kitchen area and adjacent spaces without fire detection for 6 hours until morning technician arrival.
Decision Point: October 2019
Emergency facilities meeting convened.
Present:
- Facilities Director
- Hospital Safety Officer
- Director of Plant Operations
- Fire Protection Contractor Representative
- Risk Management Director
Discussion summary:
“We’ve spent $37,000 on this fire alarm system over the last five years. Troubles are increasing. False alarms are increasing. We’re about to start paying false alarm fines. Parts availability is becoming a problem—last service call took two weeks to source a replacement detector base. The system is 23 years old.
We need to decide: Continue repairing this system, or replace it?”
Contractor assessment:
“Your panel is obsolete. Replacement parts are sourced from salvage. The detectors are approaching end of service life—should be replaced in 2-3 years regardless of other issues. The conventional technology means every trouble requires hours of troubleshooting because the panel can’t tell you which specific device has the problem.
You could continue repairing. But I estimate you’ll spend $8,000-10,000 annually on service calls for the next several years, plus detector replacement costs when needed, plus risk of panel failure requiring emergency replacement.
Or we can plan a phased replacement over 18-24 months, upgrading to addressable system that identifies specific devices, provides much better diagnostic information, and integrates with your building automation and nurse call systems.”
Risk management perspective:
“False alarms are affecting our relationship with the fire department. If we get cited for excessive false alarms, that goes on record. It affects our accreditation status potentially. And having zones out of service for hours while waiting for troubleshooting creates liability exposure.
From risk management standpoint, we need reliable fire protection. This system isn’t reliable anymore.”
Decision:
Proceed with replacement planning. Target: Begin installation Q2 2020, complete by Q4 2021. Budget: Allocate $250,000 over two fiscal years.
—
Planning: The 6-Month Process
November 2019 – April 2020
#
Design Phase
Hired: Fire protection engineering firm for system design.
Requirements gathering:
Life safety:
- NFPA 101 healthcare occupancy requirements
- State healthcare facility regulations
- Local fire code amendments
- Joint Commission accreditation standards
Operational:
- Integration with nurse call system (alarm notifications to nursing stations)
- Integration with building automation (HVAC control, door release)
- Integration with access control (emergency door unlocking)
- Future capability for mass notification
Specific challenges:
Hospital remains fully operational during installation:
- Patient care cannot be interrupted
- Certain areas (ICU, ER, surgery) have restricted work windows
- Infection control protocols must be followed
- Noise restrictions during night hours
Existing building constraints:
- 1970s construction—original building
- 1996 addition—current fire alarm location
- 2010 renovation—third wing
- Each area has different ceiling types, access methods, and architectural considerations
Detection requirements:
- Patient rooms: Smoke detection (meets healthcare requirements)
- Corridors: Smoke detection every 30 feet on center (NFPA 101)
- Mechanical rooms: Heat detection
- Kitchen: Rate-of-rise heat detection (smoke detectors false alarm from cooking)
- Storage areas: Smoke detection
- Special spaces (MRI, surgical): Specific detection types based on use
Notification requirements:
- Patient rooms: Visual notification (strobes) only (per NFPA 101—no audible in sleeping rooms)
- Corridors: Voice evacuation with visual notification
- Public areas: Voice evacuation with visual notification
- Staff areas: Audible and visual notification
#
System Selection
Chosen system: Addressable fire alarm with voice evacuation capability.
Why addressable:
- Individual device identification (panel shows “Smoke Detector 247, Room 302” not “Zone 4”)
- Device-level diagnostics (panel reports “Detector needs cleaning” before it false alarms)
- Faster troubleshooting (pinpoint device with problem in seconds)
- Better reporting capabilities (detailed event logs for accreditation inspections)
Device count:
- Smoke detectors: 340
- Heat detectors: 85
- Manual pull stations: 45
- Voice evacuation speakers: 180
- Visual notification (strobes): 190
- Duct detectors: 12
- Total addressable points: 852
#
Budget Development
Initial contractor estimate: $285,000
Value engineering session:
- Use existing conduit where possible (reduces installation labor): -$15,000
- Reduce panel redundancy (single main panel instead of two): -$8,000
- Defer mass notification integration to future phase: -$12,000
Revised budget: $250,000
Breakdown:
- Equipment (panels, devices, notification): $95,000
- Installation labor: $110,000
- Engineering and design: $18,000
- Project management: $12,000
- Commissioning and testing: $8,000
- Contingency (10%): $7,000
#
Phasing Strategy
Phase 1 (June-August 2020): Administrative wing and main corridors
- Lower occupancy density
- Easier access
- Tests installation procedures and coordination
- Budget: $85,000
Phase 2 (September-November 2020): Patient care areas—North wing
- Higher complexity
- More coordination required
- Build on Phase 1 experience
- Budget: $90,000
Phase 3 (March-May 2021): Patient care areas—South wing and kitchen
- Complete remaining patient areas
- Highest-risk areas last (kitchen, mechanical)
- Budget: $75,000
Why phasing:
- Spreads budget across two fiscal years (2020 and 2021)
- Reduces project risk (problems in Phase 1 corrected before later phases)
- Maintains fire protection (existing system remains operational in areas not yet upgraded)
- Reduces disruption (smaller work areas at any given time)
#
Approval Process
January 2020: Hospital Board presentation
- Facilities Director presents project scope, budget, timeline
- Board questions about operational disruption
- Board approval: February 2020 meeting
February 2020: Fire Marshal pre-submittal meeting
- Review design approach
- Confirm code compliance strategy
- Discuss phased installation and permit process
March 2020: Permit application submission
- Design drawings
- Equipment specifications
- Installation methodology
- Phasing plan
April 2020: Permit approval received
- Start date: June 1, 2020
—
Installation: 12 Months of Coordination
Phase 1: June-August 2020
#
Week 1: Mobilization
Coordination meeting:
Present: Contractor project manager, hospital facilities director, director of plant operations, infection control coordinator, safety officer.
Topics:
- Daily schedule (work hours 7 AM – 3 PM weekdays, minimize disruptions)
- Access procedures (contractor badging, background checks complete)
- Infection control (dust containment, pathway isolation during ceiling work)
- Communication (daily morning briefing, immediate notification of issues)
Safety protocols established:
- All contractors: Background checks and health screening
- Dust-generating work: Barriers and negative pressure isolation
- Work above patient areas: After-hours only or during discharge/transfer windows
- High-traffic areas: Work during lowest census periods
#
Weeks 2-8: Installation
Process:
Morning (7:00-7:30 AM): Daily coordination meeting
- Today’s work locations
- Yesterday’s issues and resolutions
- Today’s anticipated challenges
Daily work:
- Pull wire through existing conduit where possible
- Install new conduit where necessary
- Mount devices and notification appliances
- Label all wiring
- Preliminary device testing
Challenges encountered:
Week 3: Asbestos discovery
- Ceiling tile removal reveals asbestos-containing material
- Work stop in affected corridor
- Asbestos abatement scheduled (2-week delay)
- Cost: $8,500 additional (covered by contingency)
Week 5: Conflicting electrical work
- Electrical contractor replacing lighting at same time
- Both projects need ceiling access in same area
- Resolution: Coordinated schedule (fire alarm morning, electrical afternoon)
Week 6: Device relocation request
- Stroke detector location conflicts with planned millwork installation
- On-site meeting with architect
- Device relocated 8 feet—requires fire marshal approval of revision
- Approval received same day via email
#
Weeks 9-10: Testing and Cutover
Testing procedure:
Device-by-device testing:
- Technician activates each device
- Verifies panel receives signal
- Confirms correct device identification displayed
- Tests notification in that zone
- Documents results
System integration testing:
- HVAC shutdown on alarm (verified)
- Door holder release (verified)
- Nurse call system notification (verified—appears on nursing station screens)
- Building automation interface (verified—BAS receives alarm information)
Functional testing:
- Smoke detector sensitivity testing (all devices within acceptable range)
- Notification audibility testing (meets NFPA 72 requirements)
- Voice intelligibility testing (speech intelligible in all spaces)
- Battery backup testing (system operates 24 hours on battery)
Cutover: August 15, 2020
Process:
1. Place old system out of service in Phase 1 areas
2. Activate new system
3. Final verification testing
4. Fire watch eliminated (new system fully operational)
5. Old system devices in Phase 1 areas removed over following week
Phase 1 Results:
- Completed: On budget, 2 weeks behind schedule (asbestos delay)
- Device count: 285 devices installed
- No patient care disruption
- Zero infection control incidents
- Lessons learned: Document for Phase 2 improvements
—
Phase 2: September-November 2020
#
Improvements Based on Phase 1 Experience
Better scheduling:
- Pre-identify all ceiling areas requiring asbestos inspection
- Abatement completed before fire alarm work begins
- Eliminates mid-project delays
Enhanced coordination:
- Weekly look-ahead meetings with all trades
- Shared access schedule posted in facilities office
- Reduces conflicts with other contractors
Refined infection control:
- Improved dust barriers based on infection control feedback
- Better communication with nursing staff about work areas
- Enhanced monitoring of work above patient care areas
#
Installation: Weeks 1-10
Similar process to Phase 1 but with improvements.
Notable difference: Patient care areas require more sensitivity.
Specific coordination:
ICU coordination:
- Work scheduled during lowest census days (identified through census data analysis)
- Critical patients transferred before ceiling work begins
- Work above ICU completed in single day (Saturday) rather than spreading across week
Surgery coordination:
- Zero tolerance for work during surgical cases
- Notification appliance installation scheduled during surgery block downtime
- Preliminary wiring completed without entering surgical spaces
- Final device installation during dedicated shutdown day (arranged months in advance)
#
Challenges Phase 2
Week 4: Device compatibility issue
- New smoke detector bases don’t fit existing back boxes (different mounting pattern)
- Affects 30 devices
- Resolution: New back boxes installed (1-week delay, $2,400 additional cost)
Week 7: Nurse call integration complexity
- Voice evacuation messages appearing on nurse call screens but not formatted correctly
- Programming issue between systems
- Two days troubleshooting with nurse call vendor
- Resolution: Software update on nurse call side
#
Cutover: November 20, 2020
Phase 2 areas activated. Old system disconnected in those zones.
Cumulative progress:
- 570 of 852 devices now on new system (67%)
- Old system serving only remaining South wing
- Maintenance costs already declining (Phase 1 and 2 areas: Zero troubles since installation)
—
Phase 3: March-May 2021
#
The Final Phase
Remaining areas:
- South wing patient rooms
- Kitchen and dietary services
- Mechanical rooms and utility areas
- Connection to main building entry
Complexity factors:
Kitchen/dietary:
- Cannot shut down food service (hospital cafeteria serves staff, visitors, patients)
- Detection type critical (heat detection to prevent false alarms)
- Exhaust hood detection requires coordination with mechanical contractor
- Work scheduled during lowest meal service periods
Mechanical rooms:
- HVAC equipment sensitive to dust and disruption
- Some mechanical rooms serve critical areas (can’t be shut down)
- Detection must not false alarm from normal equipment operation
- Access challenging (confined spaces, high temperatures)
#
Installation: Weeks 1-12
Kitchen challenges:
Week 2: Hood suppression integration
- Kitchen hood has separate suppression system (Ansul system)
- Fire alarm must interface with hood suppression
- Required bringing in hood suppression contractor for coordination
- Integration testing more complex than anticipated
- 3-day delay for proper testing and verification
Week 5: Detection type optimization
- Initial heat detectors in kitchen too sensitive
- Multiple false alarms during cooking operations
- Consulting with fire marshal on detector placement alternatives
- Moved some detectors further from cooking equipment
- Changed some to higher-temperature-threshold detectors
- Resolution successful—no false alarms after adjustment
Mechanical room challenges:
Week 7: Confined space procedures
- Several mechanical rooms require confined space entry procedures
- Slows installation significantly (safety attendant required, air monitoring, permits)
- Schedule adjustment—these rooms take 3x longer than anticipated
- Additional labor cost: $3,200
Week 9: Heat and noise
- Boiler room ambient temperature 95°F
- Work duration limited to 30-minute intervals per safety requirements
- Ear protection required (noise levels above 90 dB)
- Installation extends additional week
#
Final Testing and Cutover
Comprehensive system testing: May 15-25, 2021
Building-wide integrated test:
- Test notification coverage throughout entire building
- Verify all HVAC interfaces (shutdown on alarm)
- Test all door releases and magnetic door holders
- Verify elevator recall operation
- Test nurse call integration across all units
- Confirm building automation interface operational
Voice evacuation intelligibility:
- Professional acoustic testing in representative spaces
- All areas achieve minimum 0.5 CIS (Common Intelligibility Scale) per NFPA 72
- Several speakers repositioned to improve coverage
Fire department walkthrough: May 20, 2021
- Fire marshal final inspection
- Fire crews familiarized with new system and annunciator panel locations
- Emergency responder documentation provided
Final cutover: May 28, 2021
Old fire alarm system completely decommissioned. All wiring removed from service. Old panel removed (will be disposed of properly).
Project completion:
- Total duration: 24 months from decision to final cutover
- Total cost: $254,800 (within 2% of revised budget)
- Schedule: 4 weeks longer than planned (due to unforeseen challenges)
- Disruption incidents: Zero patient care interruptions
—
After: The New Reality
June 2021 – Present
#
Immediate Changes
Trouble calls:
2021 (7 months with new system): 2 trouble calls
- Both addressed within 24 hours
- Both identified specific devices (detector needed cleaning, one pull station with low battery)
- Total service cost: $380
Compare to 2019 (with old system): 31 trouble calls, $8,500 cost
False alarms:
2021 (7 months): 0 false alarms
2022 (full year): 1 false alarm (construction dust despite containment)
2023 (full year): 0 false alarms
Compare to 2019: 8 false alarms
#
Operational Benefits
Faster troubleshooting:
Old system trouble:
- “Zone 4 Trouble”
- Technician physically inspects 60+ devices
- 4 hours average troubleshooting time
- $480 service call
New system trouble:
- “Detector 302 Dirty”
- Technician goes directly to that device
- 20 minutes to clean detector
- $95 service call (when outside contracted maintenance visits)
Better information for fire department:
Old system: Alarm in “Zone 7” (kitchen area—20,000 square feet, 4 different spaces)
New system: “Smoke Detector 715, Kitchen Prep Area, First Floor North”
Fire department arrives knowing exactly where to go. Response efficiency improved.
Nurse call integration value:
When fire alarm activates, nursing stations automatically display:
- Which device activated
- Location description
- Time of activation
Nursing staff can inform responding fire department immediately about fire location, any patients requiring evacuation assistance in that area, and whether area is occupied.
#
Maintenance Cost Comparison
Annual maintenance costs:
Old system (final years):
- 2017: $4,800
- 2018: $6,400
- 2019: $8,500
New system:
- 2021: $2,100 (contracted quarterly maintenance)
- 2022: $2,100
- 2023: $2,200
Three-year savings: $19,400
Projected 10-year savings: $65,000-75,000
#
Diagnostic Capabilities
Panel now provides:
Device-specific status:
- “Detector 245 dirty—clean within 30 days”
- “Detector 189 approaching sensitivity limit—replace soon”
- “Pull station 032 battery low”
Historical data:
- Which devices activate most frequently (identifies problem areas)
- Trouble frequency by device (identifies failing devices before complete failure)
- Environmental conditions affecting detectors (temperature, humidity at detector locations)
Preventive maintenance improved:
Old system: Reactive (fix things when they break)
New system: Predictive (identify problems before failures occur)
#
Risk Management Perspective
Risk Manager statement (2023 annual review):
“Fire alarm system replacement has substantially reduced our liability exposure. We’ve eliminated false alarm citations. Our accreditation inspections show zero fire alarm deficiencies. Most importantly, we have confidence that the fire alarm system will work when needed. The old system had become a compliance liability. The new system is a risk mitigation asset.”
#
Financial Return on Investment
Project cost: $254,800
Annual savings:
- Reduced maintenance: $5,000-6,000 annually
- Avoided false alarm fines: $1,000-2,000 annually (conservative estimate based on 2019 trajectory)
- Reduced troubleshooting labor: $2,000-3,000 annually
- Total: $8,000-11,000 annually
Simple payback period: 23-32 years
“That doesn’t sound impressive. Why was this worth doing?”
Unquantified benefits:
- Avoided emergency replacement (would have cost $350,000+ when old system finally failed catastrophically)
- Improved accreditation compliance (difficult to quantify but affects Medicare/Medicaid reimbursement)
- Reduced liability exposure (false alarm during real emergency, system failure during fire)
- Better operational efficiency (faster response to troubles, better information for fire department)
- Technology platform for future enhancements (mass notification, advanced integration)
Risk management perspective on ROI:
“You can’t calculate ROI on fire protection by looking at maintenance costs. The real ROI is avoiding the one catastrophic fire where inadequate fire alarm contributes to poor outcome. That scenario—even once in 50 years—costs orders of magnitude more than $250,000 in liability, reputation damage, and regulatory consequences.”
—
Lessons: What We Learned
For Other Healthcare Facilities Considering Replacement
#
Lesson 1: Don’t Wait for Complete Failure
Facilities director reflection:
“We waited too long. We should have started this project in 2017 when we saw maintenance costs rising. By waiting until 2019, we dealt with false alarm fines, zones out of service, and relationship strain with fire department. Earlier action would have been less stressful and less risky.”
Recommendation: Begin replacement planning when system reaches 15-18 years old, not waiting until 20+ years when reliability problems severe.
#
Lesson 2: Phasing is Essential for Occupied Facilities
Project manager perspective:
“Trying to replace the entire system at once would have been impossible without shutting down portions of the hospital. Phasing allowed us to maintain operations, spread budget across fiscal years, and learn from early phases to improve later work.”
Recommendation: Plan 18-24 month phased projects for occupied healthcare facilities. Faster isn’t better if it disrupts patient care.
#
Lesson 3: Infection Control Coordination is Critical
Infection control coordinator:
“Fire alarm contractor understood they were working in healthcare environment. They followed our protocols, responded to our concerns, and adjusted methods when we identified issues. This prevented any infection control incidents during 12 months of construction.”
Recommendation: Involve infection control from project beginning. Their requirements are non-negotiable and affect project methodology significantly.
#
Lesson 4: Integration Planning Requires Extra Time
IT director perspective:
“We underestimated complexity of integrating new fire alarm with existing nurse call and building automation systems. Programming, testing, and troubleshooting these interfaces took longer than physical installation. Build extra time into schedule for integration work.”
Recommendation: If new fire alarm integrates with other systems, add 20-30% time contingency specifically for integration testing and troubleshooting.
#
Lesson 5: Hidden Conditions are Inevitable
Contractor project manager:
“We found asbestos, conflicting back box sizes, confined space requirements we hadn’t anticipated, and various other surprises. That’s normal in renovation work. We included contingency budget and schedule float specifically for these unknowns.”
Recommendation: Include 10-15% budget contingency and schedule float. Will probably use most or all of it.
#
Lesson 6: Communication Prevents Problems
Hospital safety officer:
“Daily morning meetings kept everyone informed. When issues arose, we addressed them immediately rather than discovering problems days later. Communication investment paid off in smoother project execution.”
Recommendation: Establish regular communication cadence and stick to it even when seems redundant.
#
Lesson 7: Value Engineering Must Maintain Quality
Facilities director budget perspective:
“We reduced project cost by $35,000 through value engineering. But we were careful not to compromise core functionality or quality. We deferred nice-to-have features to future phases rather than cheapening the base system.”
Recommendation: Value engineer scope and timing, not quality. Cheap fire alarm system is expensive in long run.
—
Epilogue: Three Years Later
Current Status (2024)
System age: 4 years
Total troubles since installation: 6 (all resolved within 24-48 hours)
False alarms since installation: 1 (construction-related)
Annual maintenance cost: $2,200
Staff confidence in fire alarm reliability: High
Facilities director final reflection:
“Looking back, I wish we’d done this sooner. We spent five years managing an increasingly unreliable system, dealing with false alarms, paying escalating maintenance costs, and worrying about catastrophic failure. The new system works quietly in the background doing its job. That’s what fire protection should do—be there when needed, stay out of the way otherwise.
Was $250,000 a significant investment? Yes. Was it worth it? Absolutely. We have reliable fire protection, better building integration, reduced operating costs, and eliminated a major compliance and liability concern. Most importantly, we have confidence that if a fire occurs, this system will detect it, notify occupants, alert fire department, and interface with building systems appropriately.
That confidence is worth more than the money we spent.”
—
Key Takeaways
Fire alarm system replacement in occupied facilities requires:
Careful planning – Six months of design, budgeting, and coordination before installation begins
Phased approach – 18-24 months for healthcare facilities maintains operations and spreads budget
Infection control coordination – Healthcare-specific protocols are non-negotiable
Integration complexity – Allow extra time for building system interfaces
Contingency planning – Budget and schedule buffers for unexpected conditions
Ongoing communication – Regular meetings prevent problems and keep stakeholders informed
Long-term perspective – ROI measured in decades and risk reduction, not just maintenance savings
The journey from “Zone 4 Trouble” to “Detector 302 Dirty” represents more than technology upgrade. It represents transformation from reactive crisis management to proactive reliable fire protection.
—
Your Facility’s Story
Every building has different needs, constraints, and priorities. Healthcare facilities face unique challenges with 24/7 operations, infection control, and patient safety. But the fundamental question remains the same:
Is your fire alarm system providing reliable protection, or has it become liability you’re managing?
If you’re experiencing increasing troubles, rising maintenance costs, false alarm problems, or simply have aging equipment approaching end of service life, it’s time to evaluate options.
Need help assessing your fire alarm system condition and developing replacement strategy appropriate for your facility? [Talk to an expert](/contact-us) at 48fire who understands the complexities of replacing fire alarm systems in occupied buildings, can develop phased approaches minimizing disruption, and provides honest assessment of whether repair or replacement makes sense for your specific situation.
The story doesn’t have to include emergency replacement during system failure. With proper planning, fire alarm modernization can be managed project that improves reliability, reduces costs, and eliminates worry about critical fire protection equipment.